Study Identifies Key Barriers and Facilitators for Medications to Treat Opioid Use Disorders in U.S. Jails
Findings from JCOIN’s Chestnut Health Systems Clinical Research Center
Transitioning to the community following incarceration is a particularly high risk for individuals with opioid use disorder (OUD), especially during the first two weeks of release. Substantial evidence shows that initiating medications for opioid use disorder (MOUD) during incarceration and continuation after release reduces the risk of overdose death, recidivism, and adverse health and social outcomes.1-3 Jails can play a pivotal role in addressing OUD by providing continuity of MOUD treatment and care in the community. However, many barriers prevent the widespread adoption of evidence-based OUD treatment practices in justice settings.
A recent study by Drs. Christy Scott, Christine Grella, Michael Dennis and their team at Chestnut Health Systems identified significant barriers and facilitators that impede access to MOUD in U.S. jails. Structured interviews were completed between December 2019 and February 2021 with representatives from 185 jails in counties that the opioid epidemic has most heavily impacted. Selected counties accounted for half of all opioid-related deaths nationally and had significantly higher rates of opioid-related overdose deaths per 100,000 people than the U.S. overall.
Results
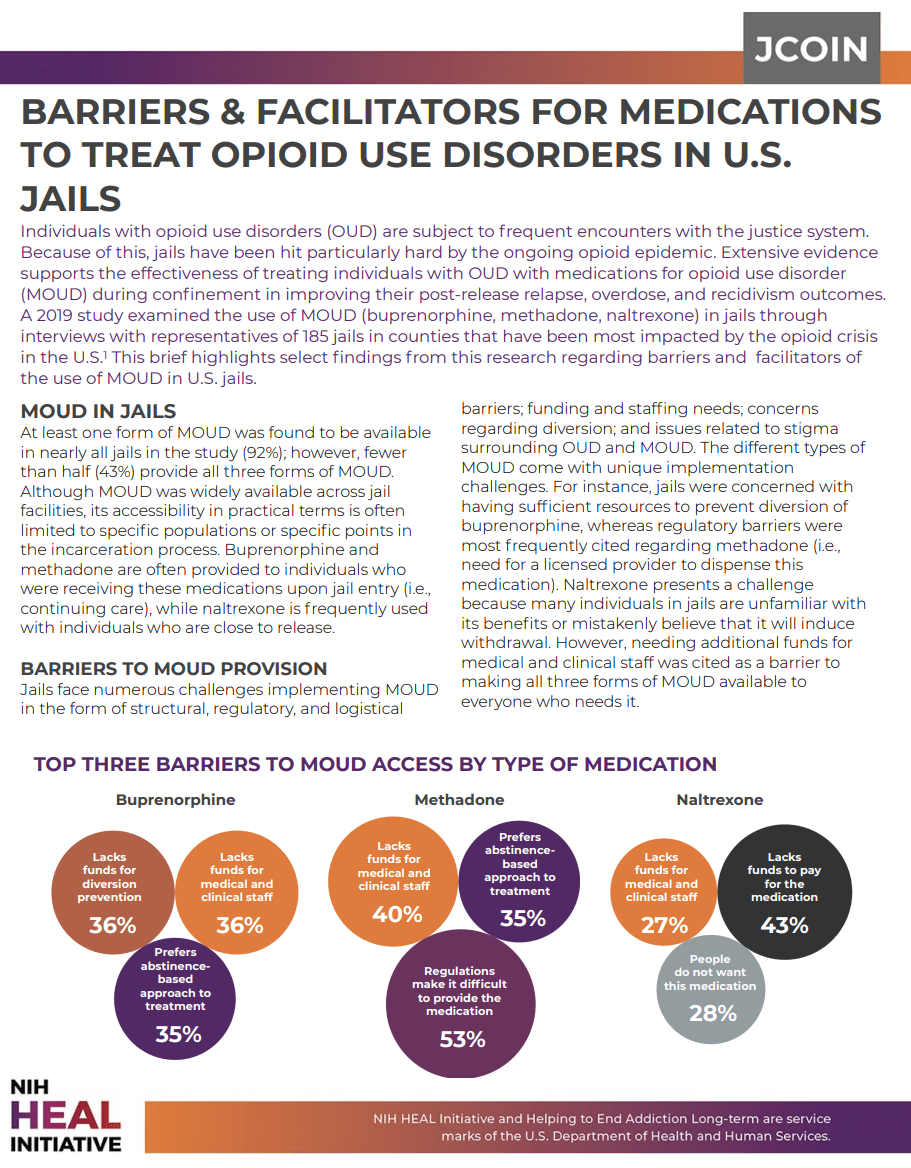
Findings show that the majority of jails provide at least one form of MOUD (92%), yet only 43% provide all three forms of MOUD (methadone, buprenorphine, and naltrexone). Even when available, most jails limit provision of MOUD to certain populations, for example pregnant women or those who are already using it; only 20% provide MOUD to anyone who is assessed with OUD., Jails reported several challenges affecting their ability to expand the accessibility of these medications. The most prominent concern among respondents (90.8%) was the need for additional funding to help purchase and administer MOUD-related services, hire and train more clinical staff, prevent diversion, and access MOUD in the community.
Researchers also identified barriers by type of MOUD. In addition to needing additional funding for each medication, regulatory barriers were of most concern among jails that provide methadone; jails that provide buprenorphine reported concerns about insufficient resources to prevent medication diversion; while many jail personnel are unfamiliar with the benefits of naltrexone or mistakenly believe that it will induce withdrawal.
Needs for assistance with reentry planning and services to ensure continuity of care after release was also a top concern, with 90.3% of respondents signaling this as a significant barrier. These services include transportation to providers, funding for MOUD in the community, same-day access to MOUD upon release, navigating regulatory and insurance requirements, recovery housing, and employment opportunities.
Other challenges include addressing stigma, which often impedes access to and retention in services, and educating stakeholders about OUD and evidence-based treatment, such as correctional, judicial, political, and community-based stakeholders and the general public. Findings also indicate a need and interest from jails to receive further training and technical assistance to increase their ability to provide OUD services.
Due to the selection criteria of the counties, study findings may not generalize to jails in areas less impacted by the opioid epidemic at the time the study was conducted. Participating jails in the study had significantly higher rates of opioid-related overdose deaths. The study team noted that these areas may have implemented aggressive policies to address their highly visible opioid-related problems, including expansion of OUD-related services.
Key Takeaways
What this means for future research
Limited availability of MOUD in correctional and community settings can have devastating consequences and place individuals with OUD re-entering society at higher risk of relapse, rearrest, reincarceration, and experiencing a fatal drug overdose. This study highlights critical barriers and challenges that impact jails' ability to implement or expand access to MOUD in their facilities. Findings emphasize that jails, in particular, are in great need of additional funding for MOUD and clinical capacity, support with re-entry services to ensure continuity of care in the community, and help addressing stigma and negative attitudes toward MOUD.
This summary highlights select findings from the 2022 publication, Availability of best practices for opioid use disorder in jails and related training and resource needs: findings from a national interview study of jails in heavily impacted counties in the U.S.
This summary is based on the findings from the following publication:
Scott, C. K., Grella, C. E., Dennis, M. L., Carnevale, J., & LaVallee, R. (2022). Availability of best practices for opioid use disorder in jails and related training and resource needs: findings from a national interview study of jails in heavily impacted counties in the U.S. Health & justice, 10(1), 36. https://doi.org/10.1186/s40352-022-00197-3
References
- Degenhardt, L., Larney, S., Kimber, J., Gisev, N., Farrell, M., Dobbins, T., Weatherburn, D. J., Gibson, A., Mattick, R., Butler, T., & Burns, L. (2014). The impact of opioid substitution therapy on mortality post-release from prison: retrospective data linkage study. Addiction (Abingdon, England), 109(8), 1306–1317. https://doi.org/10.1111/add.12536
- Evans, E. A., Wilson, D., & Friedmann, P. D. (2022). Recidivism and mortality after in-jail buprenorphine treatment for opioid use disorder. Drug and alcohol dependence, 231, 109254. https://doi.org/10.1016/j.drugalcdep.2021.109254
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on Medication-Assisted Treatment for Opioid Use Disorder, Mancher, M., & Leshner, A. I. (Eds.). (2019). Medications for Opioid Use Disorder Save Lives. National Academies Press (US). https://www.nap.edu/catalog/25310/medications-for-opioid-use-disorder-save-lives