State Pathways for Improving Pre-Release Services and Supports: Medicaid Initiatives & 1115 Reentry Waivers

Medicaid offers crucial opportunities to provide services to individuals impacted by the criminal legal system and offers a funding stream for services that can be difficult for local governments to provide. In states that have opted into Medicaid expansion, eligible incarcerated individuals are able to access pathways to Medicaid coverage via Section 1115 reentry waivers. Section 1115 of the Social Security Act enables states to apply to carry out demonstration projects testing innovative, tailored ways of meeting the needs of specific Medicaid populations. By way of Section 1115 reentry waivers, states can circumvent Medicaid’s inmate exclusion rule, which usually precludes authorizing Medicaid funding for most health services delivered while an individual is incarcerated. Reentry waivers authorize Medicaid coverage for services, including, but not limited to, substance use treatment while a person is incarcerated and case management to assist individuals in maintaining access to substance use treatment once released from incarceration.
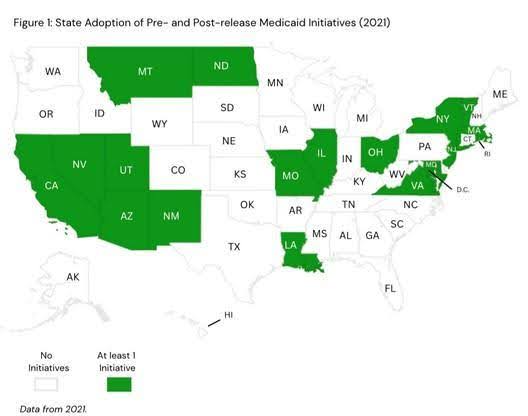 Survey data from 2021 (See Figure 1) demonstrate that the states that pursued pre- and post-release Medicaid initiatives separate from the 1115 waiver mechanism. These initiatives include Medicaid enrollment supports, pre-release provision of medications for opioid use disorder, and post-release substance use disorder treatment coordination, among others. Eighteen states and the District of Columbia adopted at least one Medicaid initiative for incarcerated individuals with a substance use disorder (Lewis et al. 2024). Reentry waiver approvals since 2023—when CMS released reentry waiver guidance—mark an important increase in federally matched state efforts to expand access to healthcare and supportive services for this population.
Survey data from 2021 (See Figure 1) demonstrate that the states that pursued pre- and post-release Medicaid initiatives separate from the 1115 waiver mechanism. These initiatives include Medicaid enrollment supports, pre-release provision of medications for opioid use disorder, and post-release substance use disorder treatment coordination, among others. Eighteen states and the District of Columbia adopted at least one Medicaid initiative for incarcerated individuals with a substance use disorder (Lewis et al. 2024). Reentry waiver approvals since 2023—when CMS released reentry waiver guidance—mark an important increase in federally matched state efforts to expand access to healthcare and supportive services for this population.
Nine of the eighteen states (AZ, CA, IL, MD, MA, MT, NM, UT, VT) have since received approval for their reentry waivers.
Section 1115 Reentry Waivers
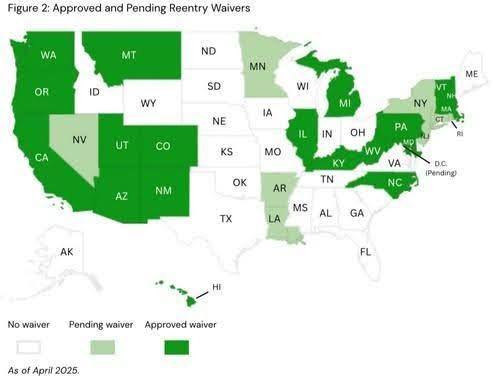 The Reentry 1115 waiver was introduced in 2023, and as of April 2025, the Centers for Medicare and Medicaid Services (CMS) has approved 19 Reentry Section 1115 Demonstrations, with nine states pending approval (See Figure 2). These waivers focus on Medicaid program improvements and innovations aimed at more effectively meeting the health and social needs of people transitioning out of prisons, jails, and youth detention facilities. Reentry waiver benefits aim to improve continuity and quality of care, allowing Medicaid to cover a specific package of pre-release services.
The Reentry 1115 waiver was introduced in 2023, and as of April 2025, the Centers for Medicare and Medicaid Services (CMS) has approved 19 Reentry Section 1115 Demonstrations, with nine states pending approval (See Figure 2). These waivers focus on Medicaid program improvements and innovations aimed at more effectively meeting the health and social needs of people transitioning out of prisons, jails, and youth detention facilities. Reentry waiver benefits aim to improve continuity and quality of care, allowing Medicaid to cover a specific package of pre-release services.
Reentry Waiver Variation
Reentry waivers vary depending on states’ interest in and capacity for providing a range of services. Waivers also vary based on eligibility criteria for beneficiaries, the timing at which pre-release coverage initiates (anywhere from 30-90 days prior to release), and which carceral settings will participate in the delivery of demonstration benefits. Some states offer the minimum service package needed for CMS approval, and others extend coverage for additional services identified as crucial for incarcerated individuals’ other, more common health and social needs.
Minimum Package of Services
- Case management to identify and address physical, behavioral, and health-related social needs
- Medication-assisted treatment for all types of substance use disorder
- 30-day supply of all prescribed medications (deemed clinically necessary) upon release
Additional Services
- Physical, behavioral, and dental health screenings and clinical consultation
- Diagnostic services (e.g., sexually transmitted infections, HIV, diabetes, hypertension)
- Peer & community health worker supports Family planning services & supplies, Hepatitis C treatment
- Provision of durable medical equipment (e.g., wheelchairs, oxygen equipment) upon release
Reentry Waivers and Expanding Coverage
In order to receive CMS approval for their waivers, states must adopt a policy suspending an individual’s Medicaid coverage while they are incarcerated, as compared to the traditional termination of benefits. If states do not adopt this suspension policy upon applying for a reentry waiver, they are expected to do so within two years following waiver approval. Other policy options states may choose to include in their waivers are standardizing pre-release Medicaid enrollment and renewal for all eligible individuals and pre-release outreach to identify all interested Medicaid-eligible individuals. Waiver services can include assigning individuals a Medicaid application counselor, and/or conferring presumptive eligibility for people who are likely Medicaid-eligible and in need of immediate access to care during a short-term incarceration period. Waivers can be a key mechanism for expanding access to Medicaid coverage, both during and after incarceration.
How States Apply for Waivers
States can either amend their existing 1115 waivers to incorporate the Reentry demonstration or they can submit a new, separate 1115 demonstration application. In both cases, states will need to provide detailed information about eligible beneficiaries, types of pre-release services offered, participating carceral settings, and timelines for pre-release service delivery. States are also expected to outline anticipated challenges and means of addressing them in a required implementation plan. An added benefit of the 1115 waivers is that states can request funding for their Medicaid Management Information Systems. This can assist with demonstration evaluation efforts, data-sharing, and communication across reentry stakeholders. CMS offers various publicly available application and implementation plan templates to streamline the process: www.medicaid.gov/medicaid/section-1115-demonstrations/1115-application-process
References
Center For Health Law and Policy Innovation. “Health and Reentry.” Accessed April 30, 2025. https://chlpi.org/project/health-and-reentry/
Centers for Medicare and Medicaid Services. “State Medicaid Director Letter #23-003.” Department of Health and Human Services, April 17, 2023. https://www.medicaid.gov/federal-policy-guidance/downloads/smd23003.pdf
“Health Care Transitions for Individuals Returning to the Community from a Public Institution: Promising Practices Identified by the Medicaid Reentry Stakeholder Group.” U.S. Department of Health and Human Services - Office of the Assistant Secretary for Planning and Evaluation, January 2023. https://aspe.hhs.gov/sites/default/files/documents/d48e8a9fdd499029542f0a30aa78bfd1/health-care-reentry-transitions.pdf
Hinton, Elizabeth, Akash Pillai, and Amaya Diana Published. “Section 1115 Waiver Watch: Medicaid Pre-Release Services for People Who Are Incarcerated.” KFF (blog), August 19, 2024. https://www.kff.org/medicaid/issue-brief/section-1115-waiver-watch-medicaid-pre-release-services-for-people-who-are-incarcerated/
Lewis, Cashell D., Christina Andrews, Amanda J. Abraham, Melissa Westlake, Faye S. Taxman, and Colleen M. Grogan. “State Medicaid Initiatives Targeting Substance Use Disorder in Criminal Legal Settings, 2021.” American Journal of Public Health 114, no. 5 (May 2024): 527–30. https://doi.org/10.2105/AJPH.2024.307604.
Medicaid Section 1115 Demonstrations. “Reentry Section 1115 Demonstration Opportunity | Medicaid.” Accessed April 11, 2025. https://www.medicaid.gov/medicaid/section-1115-demonstrations/reentry-section-1115-demonstration-opportunity