7 Best Practices for Using MOUD Across the Cascade of Care in Criminal Legal Settings
Findings from JCOIN’s Coordination and Translation Center (CTC)
The growing rates of substance use and overdose deaths have significantly impacted the U.S. criminal legal system. Almost half of individuals in federal facilities (Mumola & Karberg, 2006), 58% in state facilities, and 63% in county jails (Bronson, 2017) have a substance use disorder. Despite the high prevalence rates), very few individuals receive evidence-based treatment, such as medications for opioid use disorder (MOUD). Providing MOUD during incarceration and during reentry has shown to reduce overdose deaths (Degenhardt et al, 2024) and recidivism (Evans et al, 2022), and increase treatment engagement, retention, and health outcomes (National Academies of Sciences, 2019).
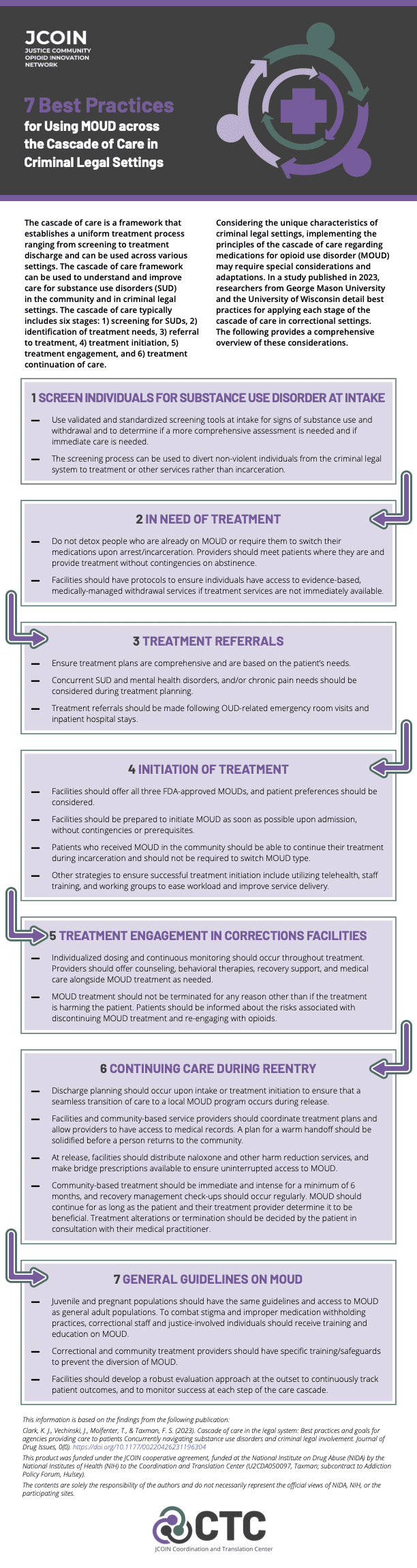
Utilizing a public health framework such as the cascade of care could help criminal legal settings improve system-level practice and treatment outcomes. The cascade of care was initially developed to measure the quality of HIV care delivery to improve survival and reduce transmission and has since been applied to other diseases. The framework establishes a uniform treatment process ranging from screening to treatment discharge and can be used to identify gaps in service delivery and implement improvements in the continuum of care for SUD. The cascade of care typically includes six stages: 1) screening for SUD, 2) identification of treatment needs, 3) referral to treatment, 4) treatment initiation, 5) treatment engagement, and 6) treatment continuation of care.
Considering the unique characteristics of criminal legal settings, implementing the principles of the cascade of care regarding MOUD may require special considerations and adaptations. In a study published in 2023, researchers from George Mason University and the University of Wisconsin detailed seven best practices and recommendations for implementing MOUD across each stage of the cascade of care in correctional settings.
The following highlights some of these considerations. Click here to download the infographic with the comprehensive list of recommendations.
- Use validated and standardized screening tools at intake for signs of substance use and withdrawal and to determine if a more comprehensive assessment is needed and if immediate care is needed.
- Do not detox people on MOUD or require them to switch their medications upon arrest/incarceration. Providers should meet patients where they are and provide treatment without contingencies on abstinence.
- Patients who received MOUD in the community should be able to continue their treatment during incarceration and should not be required to switch MOUD type.
- MOUD treatment should not be terminated for any reason other than if the treatment is harming the patient. Clients should be informed about the justification for accountability measures and the risks associated with discontinuing MOUD treatment and re-engaging with opioids.
- Community-based treatment should be immediate and intense for a minimum of six months, and recovery management check-ups should occur regularly. Treatment alterations or termination should be decided by the patient in consultation with their medical practitioner.
The cascade of care can be an effective tool in establishing effective treatment protocols and can help improve client outcomes by helping identify and address gaps in existing service delivery from admission to treatment initiation to care continuation during reentry.
This study was published in the Journal of Drug Issues and led by researchers Kendra Clark, Jessica Vechinski, Todd Molfenter, and Faye Taxman, from George Mason University and the University of Wisconsin. The study also examines the current utilization of, and goals toward, the cascade of care in 29 jails and 20 jail-affiliated community-based treatment providers. Findings suggest that 20% of sites did not provide MOUD at any point of contact with clients. Of those that provided MOUD, 20% offered all three FDA-approved MOUDs during at least one stage of incarceration, and 56% of sites tracked the progress of individuals on MOUD. During reentry, 65% of sites coordinated care with community-based treatment providers effectively. The study acknowledges that despite correctional facilities' interest in improving care, they require assistance and additional resources to expand MOUD access.
This summary is based on the findings from the following publication:
Clark, K. J., Vechinski, J., Molfenter, T., & Taxman, F. S. (2023). Cascade of care in the legal system: Best practices and goals for agencies providing care to patients Concurrently navigating substance use disorders and criminal legal involvement. Journal of Drug Issues, 0(0). https://doi.org/10.1177/00220426231196304